

It’s therefore important to have tools that facilitate high quality delivery of care and help patients feel they’re being treated as people, not statistics. Patients want to be listened to, understood, and comforted.
Providers care deeply about their patients and delivering the best care possible to them. But it seldom replicates the nuances and beauty of human connection, and that deficiency is a significant problem in health care. Technology streamlines the way we live our lives and engage with one another. Build Active Engagement and Meaningful Connection
#Virtual health care visits software
Waystar uses predictive analytics and other advanced software to help patients understand how much their insurance plans would cover and how much their out-of-pocket expenses would be prior to their appointments. Bright.md provides a “virtual physician assistant” platform that helps patients find the right care in under two minutes by answering a thorough clinical questionnaire that bases the questions it poses on the individual patient’s responses. At NYU Langone, where I work, virtual appointments are booked through Epic’s online patient portal, M圜hart, which gives physicians access to a patient’s entire clinical information.
#Virtual health care visits full
One Medical’s 1Life technology ecosystem, for example, provides physicians with summary of a patient’s care history and context-based suggestions for their care as well as access to her full electronic health record. Providing a simple, clear online estimate of what their insurance would cover and what their responsibility would be before scheduling a visit would give them the gratification of making financially-informed health care decisions.Ĭare provider organizations and startups alike have already developed tools like these. Having them complete a short app-based quiz to understand their needs and concerns before scheduling a visit would ease the friction of finding the right doctor. Making the scheduling process personalized and informative could make a great initial impression on patients. Once they meet a certain benchmark of successful telehealth visits, they could be rewarded with an invitation to an exclusive seminar. As they start the visit, a digital tip sheet could pop up to outline friendly reminders on virtual care best practices (e.g., maintain eye contact, ask personal questions to get to know the patient) and the types and methods of diagnoses that can be performed to execute a successful visit. The message could include key insights about the patient’s record and reason for her visit. Picture a platform that welcomes physicians with a warm message about their upcoming appointment with a particular patient. Studies such as Mischel’s marshmallow experiment have also shown that we’re likelier to choose instant, over delayed, gratification. Models in cognitive psychology, neuroscience, and economics indicate that humans like to avoid effort. When using technology, first impressions are informed by the effort it requires to execute tasks (compared to that of alternatives) and the instant gratification it provides. So the more compelling the first impression these tools create, the likelier patients and physicians are to engage with them. Naturally, we can assume that physicians and patients - particularly those who haven’t used telehealth before - will be skeptical about adopting it. We also tend to resist novelty the older we get. It takes milliseconds for us to make snap judgments. It’s no secret that first impressions matter. Here are three ways telehealth technologies can humanize the virtual care experience for both providers and patients. In fact, some providers have already started doing so, and startups offering solutions have begun to emerge. It will require provider organizations to invest in tools that are sensitive to human emotion.

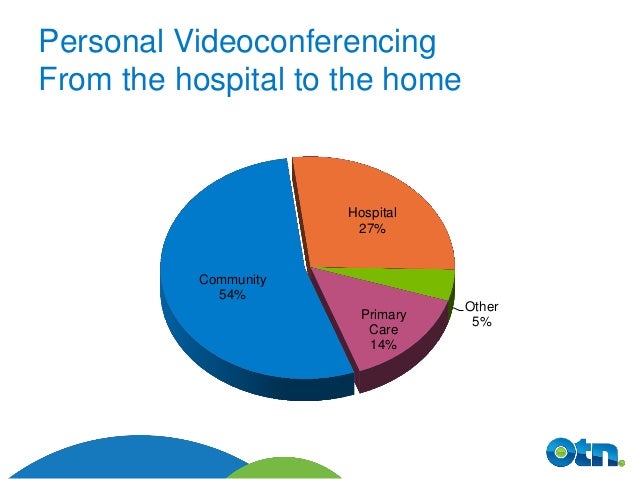
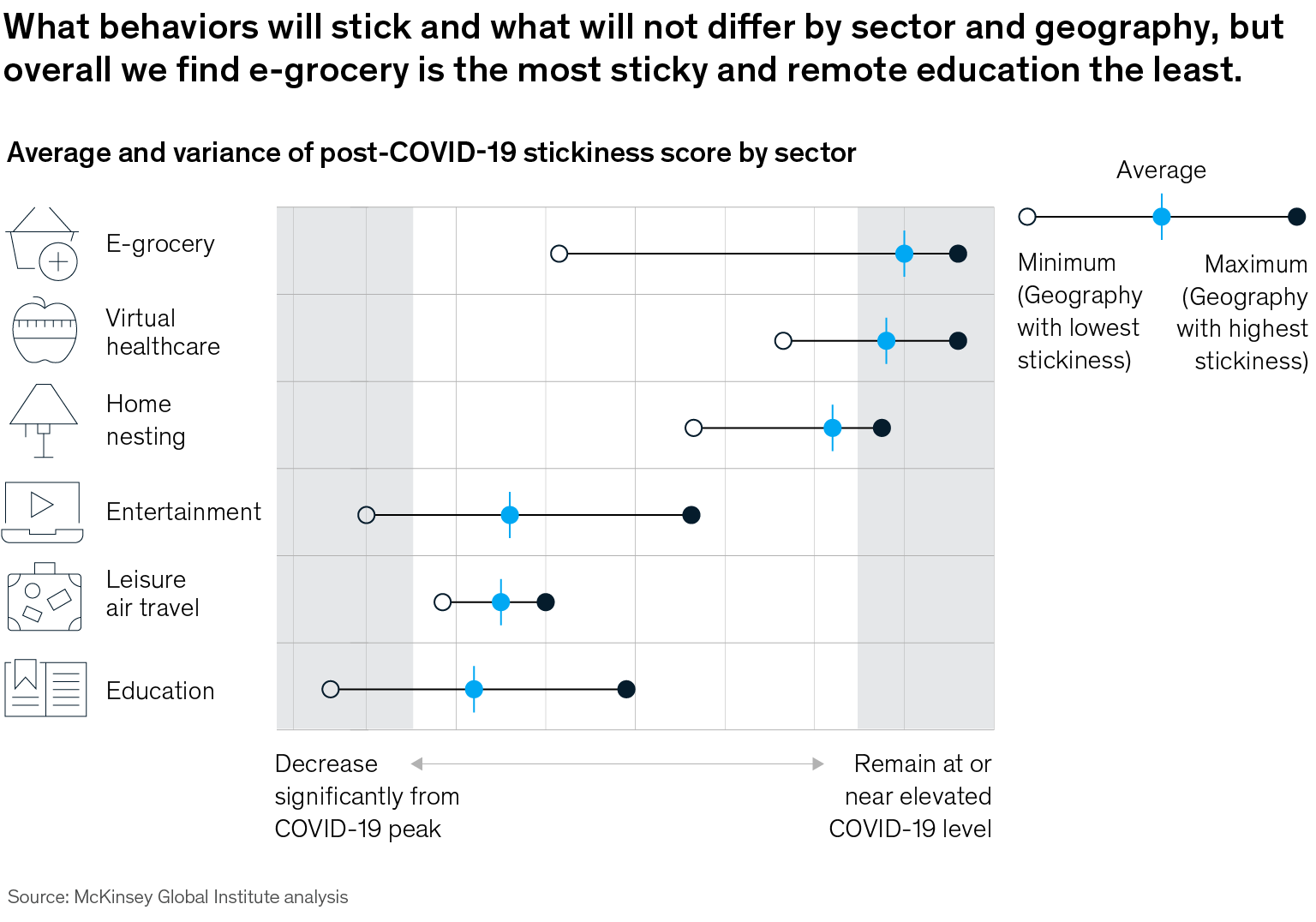
But the degree to which they do so will depend on how the experience for both groups improves. That’s because even though barriers to adoption - such as regulation, insurance coverage, and conditions requiring in-person care - will remain, provider and patient behaviors and expectations are shifting. That said, it’s safe to assume that telehealth won’t return to its pre-pandemic level, when only 8% of Americans used it. While virtual visits accounted for roughly 70% of total visits in the United States during the early stages of the outbreak, their levels dropped to about 30% towards the end of fall. To what degree will telehealth remain a dominant force in health care after the pandemic ends? That will significantly depend on how care providers invest in existing and emerging digital tools that will allow physicians and patients to build and maintain trusting relationships.


 0 kommentar(er)
0 kommentar(er)
